Abstract
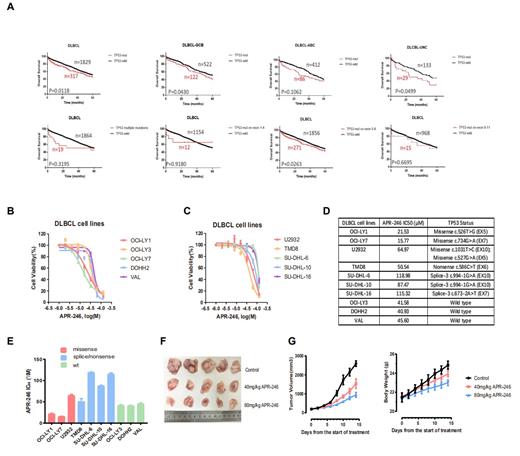
Background: Diffuse large B cell lymphoma (DLBCL) is the most common lymphoid malignancy and is characterized by its pronounced genetic and clinical heterogeneity. Although the first-line therapy (R-CHOP) improves the curability of patients with DLBCL, nearly 40% remainder ultimately undergo relapsed or refractory disease. Emerging evidence has shown that TP53 mutations correlate with the recurrence and progression of DLBCL. APR-246, also known as PRIMA-1MET, can reactivate the trans-activation of TP53 mutants by facilitating their DNA binding to target genes, making it a promising therapeutic compound for mutated TP53 carcinomas. Although APR-246 in combination with other chemicals has been applied in clinical trials for non-Hodgkin lymphoma (NHL), the efficacy and the underlying molecular mechanisms of APR-246 on DLBCL remain unclear. The arms are to investigate the TP53 mutations and the correlation of mutated TP53 with the prognosis. Furthermore, we evaluated the effect of APR-246 on DLBCL in vitro and in vivo.
Methods: Multiple datasets, including the Gene Expression Omnibus (GEO) and cBioPortal, were searched for available data for DLBCL. For evaluation of APR-246 effect on DLBCL in vitro, ten DLBCL cell lines harbouring different and representative molecular properties, especially distinct TP53 mutation status, were tested. To validate the therapeutic effect of APR-246 in vivo, NSG mice were injected subcutaneously with the DLBCL cells with TP53 mutations to establish a xenograft animal model, and then these mice received the APR-246 administration. The cell viability of DLBCL was measured post addition of APR-246. Pharmaceutical inhibition of different cell death pathways was applied to elucidate the mechanisms by which APR-246 functions.
Results: Total 2204 patients with DLBCL were evaluated, of which nearly 15% contained TP53 mutations. The missense mutation of TP53 was up to 76% and mutations occurring in the DNA binding domain (DBD) was about 90%. Patients with TP53 mutations had poor OS (p=0.0118). Further, we found that patients with TP53 mutations in GCB and UNC subtypes exhibited inferior OS (p=0.043; p=0.049, respectively), but no in ABC subtype. Notably, TP53 single mutations located in the DBD (exon 5-8) led to an unfavorable survival (p=0.0263), while patients carrying TP53 multiple mutations and single mutations in other domains exhibited no difference in survival time than those with wild-type TP53. APR-246 induced the cell death in a dose dependent manner for all DLBCL cell lines. DLBCL cells with TP53 missense mutations in the DBD were the most sensitive to APR-246 than those with intact or other types of mutated TP53. APR-246 mediated the cell death via p53-dependent ferritinophagy for DLBCL cells with TP53 missense mutations in the DBD. In addition, APR-246 also induced the ferroptosis for other DLBCL cells harbouring wild type TP53 and other forms of TP53 mutations.
Conclusions: Nearly 15% of patients with DLBCL harbouring TP53 mutations had inferior prognosis than those with wild-type TP53. Patients with TP53 single mutations occurred in the DBD (exon 5-8) showed poorer prognosis than those with TP53 multiple mutations and single mutations in other domains. APR-246 induced the cell death of DLBCL through different mechanisms, depend on different forms of TP53 mutations, which provided an evidence for clinical application of APR-246 in the treatment of DLBCL.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal